Check here every Friday for tips and tricks to help you master Nursing Pharmacology.
Today we are discussing Thrombolytics (also known as fibrinolytics)
To best understand how these medications work, let’s first discuss blood clotting/coagulation…
Our blood is flowing throughout our blood vessels at all times. So, what happens when we have an injury?
Our body acts to prevent the blood from moving out of the body through a process called coagulation. Through coagulation, blood holds firmly together at the site of injury to prevent further blood loss. Simply explained, the process looks like this:
We get an injury of some kind, be it a cut or tear in a blood vessel.
Our blood vessels vasoconstrict in an effort to reduce blood flow to that area (and thereby limit further loss).
Then, platelets are activated to create a platelet plug; platelets stick to each other and to the side of the vessel wall. Clotting factors are activated.
Fibrin, a strong, fibrous protein involved in the clotting of blood, is produced and works to create a fibrin clot. The fibrin clot is very secure and keeps the plug stable.
The ability to form clots is vital for hemostasis, but too much clotting can be detrimental…think pulmonary embolism, myocardial infarction, ischemic stroke. When clots form we can administer medications called thrombolytics to help dissolve the clot.
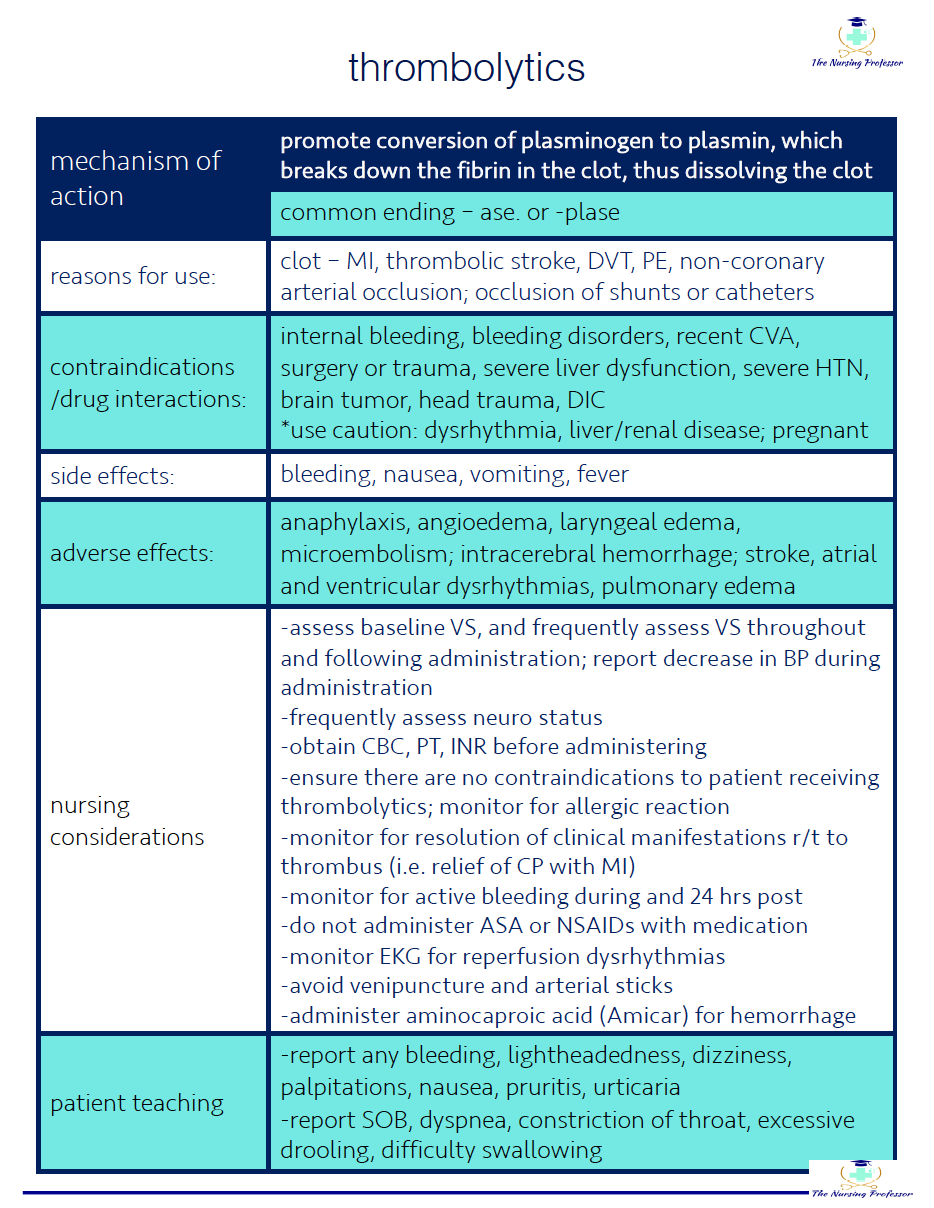
Thrombolytics work by converting plasminogen to plasmin. Plasmin lyses clots by breaking down the fibrinogen and fibrin contained in the clot.
Thrombolytics are sometimes referred to as “clot-busters” because they do just that, bust-up or dissolve the clot causing the issue.
so…If that’s how they work and what they do, in what instances would they be useful?
myocardial infarction, acute ischemic stroke, venous thrombosis, pulmonary embolism, arterial thromboembolism
Other useful info about :
· common ending: -ase or -plase
· examples: tenecteplase, streptokinase, activase
· side effects: bleeding, nausea, vomiting, fever
· adverse effects: anaphylaxis, angioedema, laryngeal edema, microembolism, intracerebral hemorrhage, stroke, atrial and ventricular dysrhythmias, pulmonary edema
· nursing considerations/patient teaching:
assess baseline VS and at least every 15 minutes throughout treatment and frequently post treatment
frequently assess neuro status
obtain CBC, PT, INR before administering
ensure there are no contraindications to patient receiving thrombolytics
must be administered within appropriate time-frame from symptom onset (i.e. for ischemic stroke must be administered within 4.5 hours of symptom onset)
monitor for resolution of symptoms (i.e. patient being treated for MI should report decrease in chest pain)
report bleeding, lightheadedness, dizziness, palpitations, SOB, dyspnea, throat constriction, excessive drooling
Because these medications are highly effective and present such a high risk of bleeding, there are numerous contraindications to using thrombolytics.
some absolute contraindications for thrombolytic therapy
recent intracranial or spinal surgery
significant head injury or facial trauma
recent intracranial hemorrhage
severe uncontrolled hypertension
possible aortic dissection
ischemic stroke within 3 months
previous treatment with streptokinase within 6 months
intracranial neoplasm
some relative contraindications for thrombolytic therapy
severe hypertension
history of ischemic stroke
pregnancy
dementia
internal bleeding within past 2 - 4 weeks
prolonged CPR
Be sure to check out the cheatsheet and podcast below…